I was really torn on Vitamin D. Correlational studies linked low Vitamin D to many disease states (mostly autoimmune) However RCT failed to show any measurable improvement. I treat low vitamin D under 30 in my patients with very conservative replacement since we had no proof that it would work and to avoid any potential side effects of over-treatment. Many immunologists don’t even check the Vitamin D levels. I Personally I limited my dose to about 10,000 I.U. per week.
This new RCT could elucidate why those previous RCT’s have failed. Correcting Vitamin D levels should occur in early stages of the disease or better yet… years before the disease first onset. This makes sense for any nutritional deficiency - like Fish Oil for delaying or preventing dementia - has to be started probably like 20 years prior to onset. So given this RCT and the recently discussed
“Individual and additive effects of vitamin D, omega-3 and exercise on DNA methylation clocks of biological aging in older adults from the DO-HEALTH trial” I decided to increase my dose 5,000 I.U. daily, I was little weary of the higher dose given my mother’s history of kidney stones.
A Rare Win for Vitamin D — This Time in MS
F. Perry Wilson, MD, MSCE
[DISCLOSURES ](javascript:void(0);)| March 10, 2025
21
588
Add to Email Alerts
00:0908:34
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson from the Yale School of Medicine.
Study after study across diseases, from Alzheimer’s disease to Zika virus infection, has shown that low vitamin D level is a risk factor for bad outcomes. Seriously, I challenge you to find a disease state where there isn’t at least some data suggesting worse outcomes among people with vitamin D deficiency.
And yet, when the inevitable randomized trial of vitamin D supplementation comes around, you get nothing. It’s become a bit of a running joke on this blog — the compelling observational data shut down by the definitive randomized trial.
SUGGESTED FOR YOU
So, we have good data that low levels are associated with various problems but a failure to show that correcting those levels makes a difference. The implication is simple: It’s the classic case of correlation vs causation. Low vitamin D levels are simply correlated with bad outcomes; they don’t cause bad outcomes. It’s not actually the vitamin D that is causing the problem; people who are sick for other reasons just happen to have low vitamin D. I actually give a lecture to the med students citing just these studies to convince them that randomized trials are superior sources of evidence than observational research.
That said, science demands that we reevaluate our priors when new data arrive. And new data have arrived, in the form of a randomized trial that, for once, shows a benefit of vitamin D supplementation. In just one disease, yes. But it’s an important one: multiple sclerosis (MS).
People with lower vitamin D levels have a higher risk for MS, and of those who develop MS, those with lower vitamin D levels have worse symptoms. But that’s the case with, well, just about every disease, because lower vitamin D levels are a marker of a lot of things: poorer health overall, less sun exposure, a less varied diet, and so on. It’s a biomarker of a healthy lifestyle. So, it’s not surprising that several prior randomized trials of vitamin D supplementation in MS have been disappointing.
But a trial can be negative for a few different reasons. There’s the common one: The treatment just doesn’t work for the disease. But there are other possibilities. Maybe the treatment was given at the wrong time, or when the disease had progressed too far. Or maybe the trial simply didn’t enroll enough people to detect a reasonable signal.
Now this study, from Eric Thouvenot and colleagues, appearing in JAMA, remedies some of those prior deficits and suggests a new role for vitamin D in MS. Let’s break down how it worked.
The investigators enrolled 316 individuals with “clinically isolated syndrome” (CIS). CIS is basically the earliest possible presentation of MS, a first episode of an MS-like syndrome such as optic neuritis. Not everyone with CIS will progress to full-blown MS, but many do. So, the first special fact about this trial is they are hitting these participants early.
The second important difference from some of the prior work is the vitamin D dose. The intervention group in this trial got 100,000 international units of oral cholecalciferol every 2 weeks. This is a big dose. The vitamin D3 you get at the local vitamin store is 1000 international units; this dose is 100 times that. Even dosed less frequently, it’s a lot. That is not without risk. Supratherapeutic doses of vitamin D can cause elevated calcium levels, kidney stones, nausea, vomiting, confusion, and so on. I’ll get to whether this happened in this study in a bit.
But first, let’s look at the patient population. A fairly young group (remember, they were enrolled at the first MS-consistent symptom); the average age was around 35. Seventy percent were female and 40% were active smokers (the study was conducted in France, where smoking is more prevalent). About 20% had severe vitamin D insufficiency, a level less than 30 nmol/L. The average time to receiving either the vitamin D or placebo was about 60 days from the initial presentation. By that time, 80% of the study population had received high-dose steroid therapy, which is pretty much standard of care.
I will point out that no one in this study received disease-modifying therapy such as interferon treatments; that was an exclusion criterion. So basically, this was a population of young individuals, newly diagnosed with early MS, who were not at super high risk for progression, at least at the time the study started.
But I’m sure you want to see the results. The primary outcome of this study was “disease activity,” and you could hit that outcome in two ways. First, a relapse of symptoms. Second, the development of new or growing lesions on MRI. MS has some characteristic findings on brain scans. Participants got follow-up MRIs at 3, 12, and 24 months.
So let’s take a look at what happened.
An increase in disease activity occurred in 74% of individuals in the placebo group, compared with 60% of individuals in the vitamin D group. That’s a 14% absolute risk reduction, which is fairly impressive.
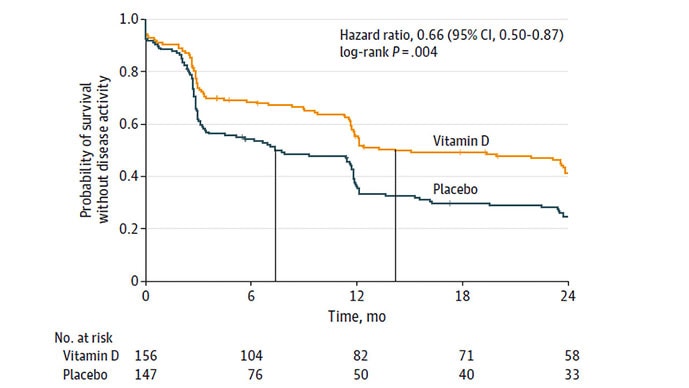
It means that you would need to treat seven individuals with early MS with vitamin D to save one person from disease progression. That’s not bad, especially for a relatively inexpensive intervention like a vitamin.
The median time to progression was significantly longer in the vitamin D group as well: 432 days vs 224 days in the placebo group. That’s around a 7-month difference.
So far, I’m impressed. But let’s take a look at some of the subgroup analyses to figure out what might really be going on here.
The first thing I want to show you is the effect of vitamin D supplementation, stratified by baseline vitamin D level. What you see here is that the supplements are dramatically more effective when the patient has vitamin D insufficiency to begin with.
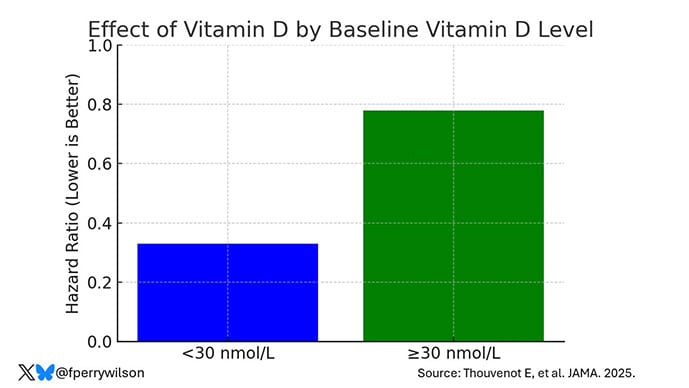
This isn’t particularly surprising, I suppose; it is fairly typical that vitamins have threshold effects. Once you hit a target — and for vitamin D something like 50 nmol/L might be reasonable — getting higher above that target doesn’t offer too much extra benefit.
The other significant finding was this: The vitamin was much more effective in people without spinal cord lesions — in other words, in people with a less severe initial presentation.
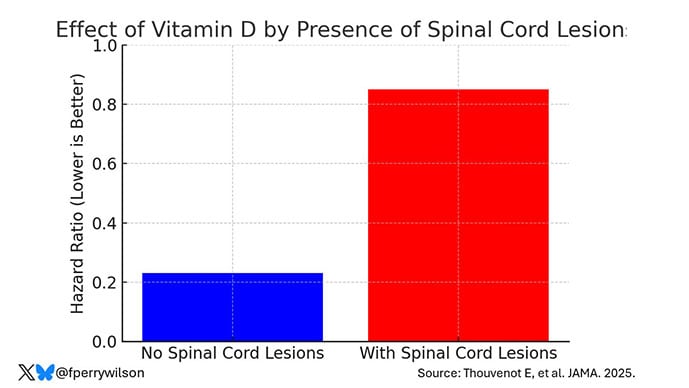
Adding to the implication that vitamin D might be best among people with less severe disease, we see that it seems to work better among the minority of people in the study who did not get intravenous steroids at the initial diagnosis. The fact that they didn’t get that therapy suggests that their presentation was milder. So, should we be giving vitamin D only to those with an initial presentation of MS that is fairly mild?
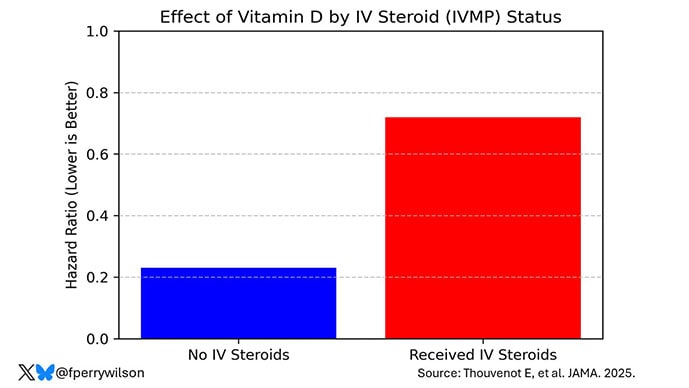
The answer to that question depends exquisitely on the risks associated with high-dose vitamin D supplementation. If it’s very risky, you’ll want to limit its use. If not, well, maybe it’s not as effective in those with worse disease but maybe it couldn’t hurt?
It seems pretty darn safe. Only two patients developed hypercalcemia during the trial, and both of them were in the placebo group. No one developed severe hypercalcemia or kidney failure. It may be a bit early to look for kidney stones, though.
Still, it’s hard to look at this trial as anything except a powerful and — to me, at least — unexpected victory for high-dose vitamin D supplementation in early MS. I think those testing vitamin D for other disease states, who look at the literature and see all those negative trials, might do well to learn some lessons from this study. If you want to design the next positive randomized trial of vitamin D, maybe start supplementation early, and when you supplement, go for big doses. Will it work for all those diseases, from Alzheimer’s to Zika? Of course not. But the first step to finding therapies that do work is to design the proper study to figure it out.