I live where odds are everything. You are in denial if you think your LDL is okay.
If you have been reading the threads, you should know that the preponderance of the evidence says your LDL is too high. Your HDL is a signal that something is wrong.
Odds are you need to be on a statin. You can bet against the house, your choice.
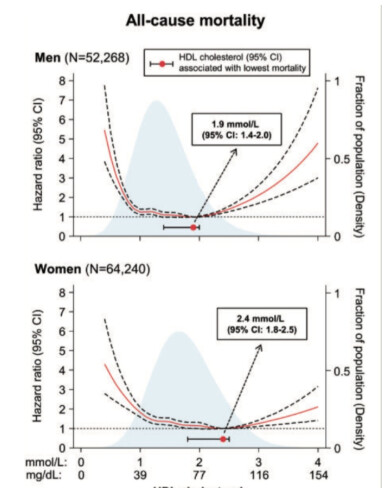
I’ve found multiple large-scale studies showing a ‘U-shaped’ risk curve. This means that both very low and very high HDL levels are linked to an increased risk of mortality, directly
contradicting the old ‘higher is better’ mantra. “The association between HDL cholesterol concentrations and all-cause mortality was U-shaped for both men and women, with both extreme high and low concentrations being associated with high all-cause mortality risk.”
"The causal leap that HDL-C was a cause of protection, not just a marker, created a testable therapeutic hypothesis: pharmacologically raising HDL-C levels should reduce cardiovascular events. This hypothesis was pursued for decades, culminating in one of the most expensive and high-profile series of failures in modern pharmaceutical history.
"High-density lipoprotein cholesterol (HDL-c) has long been referred to as ‘good cholesterol’ due to its apparent inverse relationship with future CVD risk. More recent research has questioned a causal role for HDL-c in this relationship, however, as both genetic studies and numerous large-scale randomised controlled trials have found no evidence of a cardiovascular
protective effect when HDL-c levels are raised."
“A critical revelation was that “HDL” is not a single entity. It is a highly heterogeneous (the quality of being diverse in composition) population of particles of different sizes, densities, and compositions.1 These particles can be classified broadly by density (e.g., lipid-rich HDL2 and protein-rich HDL3) 2 or charge (e.g., pre-β-HDL).”
This new paradigm leads to a practical “clinical triage” for interpreting an HDL-C result in 2025:If HDL-C is LOW (e.g., <40-50 mg/dL): Do not treat the HDL-C. Use this as a “risk enhancer”.67 The appropriate response is to be more aggressive in lowering the LDL-C target and to strongly advocate for lifestyle changes.8If HDL-C is NORMAL (e.g., 50-80 mg/dL): Acknowledge it and move on. This number is not the goal. The clinical focus remains 100% on achieving the patient’s LDL-C goal… 63 If HDL-C is “EXTREMELY” HIGH (e.g., >80-90 mg/dL): Do not celebrate. Treat this as an “abnormal level” and a red flag.13 This warrants an investigation into underlying causes, including alcohol use disorder, genetic dysfunction (like $SCARB1$), or other metabolic diseases.
https://academic.oup.com/eurheartj/article-abstract/38/32/2478/3608700?redirectedFrom=fulltext&login=false